Diabetes – Diabetic Eye Disease
Diabetic eye disease ends up affecting most people with diabetes. After 10 years of diabetes 80% of patients will have signs of diabetes that can be seen by an ophthalmologist. There are 2 common types of diabetic eye disease: diabetic retinopathy and diabetic macular oedema. Diabetic eye disease is the most common cause of blindness in the working population and is on the increase.
Diabetic Retinopathy
Diabetes affects the small blood vessels of the body. The retina (the seeing layers at the back of the eye) are supplied with oxygen and nutrients by a rich network if small blood vessels. These become damaged by high sugar levels in the blood and can become leaky or stop working altogether. The early signs of diabetic retinopathy are patches of exudates (fats and other proteins that can leak out of the damaged blood vessels) and haemorrhages (blood spots) that can be seen by an ophthalmologist (eye doctor) or an optometrist (optician) when they examine the back of the eye. As the condition progresses the small blood vessels stop working and the retina is no longer supplied with the blood that it needs. This is called retinal ischemia. The area of the retina that is starved of oxygen releases powerful factors (angiogenic factors) that can cause new vessels to grow within the jelly of the eye (the vitreous), These vessels do not grow normally and tend to break, releasing blood into the normally clear vitreous jelly in the middle of the eye. Left untreated this process leads to scar tissue and retinal detachment. The end result can be untreatable blindness.
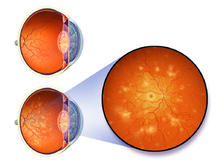
Diagram of Diabetic Retinopathy
Diabetic Macular Oedema
High quality vision relies on a very specialised small part of the retina at the centre of the eye called the macula. Diabetes can cause the fine blood vessels (capillaries) at the macula to leak. The back of the eye becomes ‘boggy’ and the fine layers of the eye needed for vision become disturbed and vision is reduced. At the Moreton Eye Group we use sophisticated equipment Optical Coherence Tomography (OCT) to measure this. Generation spectral domain OCT equipment.
The Optical Coherence Tomography (OCT) test will help with the diagnosis of a diabetic related eye disease. We may have to perform Fundus Retinal Photography and/or a Fundus Flourescein Angiography for further assessment. You will usually have been referred to us by an Optometrist, General Practitioner or other Specialist. Who will have pre-diagnosed a suspected diabetic related eye condition.
To make an appointment with one of the Ophthalmologists go the I’m a Patient page or call us on 07 3283 3488 to discuss the steps and cost for further diagnosis.
Treatment
The two surgical treatments for Diabetic Retinopathy are Laser Treatment (Photocoagulation) which is performed in any one of our three clinics. The second treatment is a Vitrectomy which is performed at the Moreton Day Hospital (MDH).
 The two treatments for Diabetic Macular Oedema are Laser Treatment (performed in our clinics) or Anti-VEGF injections performed in our clinics and/or in the Moreton Day Hospital. Our close working relationship with this state of the art facility means that your journey will be seamless from clinic to hospital, ensuring the best medical outcome for your treatment. For more information on the Moreton Day Hospital and this procedure, including costs, please see the website or call the friendly staff on 07 3487 1111.
The two treatments for Diabetic Macular Oedema are Laser Treatment (performed in our clinics) or Anti-VEGF injections performed in our clinics and/or in the Moreton Day Hospital. Our close working relationship with this state of the art facility means that your journey will be seamless from clinic to hospital, ensuring the best medical outcome for your treatment. For more information on the Moreton Day Hospital and this procedure, including costs, please see the website or call the friendly staff on 07 3487 1111.
